cN+ = pN+? – The future of prostate cancer staging
By Ass. Prof. Jeremy Grummet (Melbourne, AU), Director of Clinical Research in Urology Alfred Health
This article reflects the highlights of the lecture Ass. Prof. Jeremy Grummet will be giving during “Thematic Session 14 – Guideline Session II: Prostate cancer – cN+ in newly diagnosed patients” at EAU21 Virtual. This session takes place in Virtual room 2 on Sunday 11 July, 15.00 – 16.00 CEST.
cN+ = pN+? Or, in English, does clinical lymph node (LN) positivity equal pathological node positivity? Well, generally speaking, the answer is: yes. Regardless of the imaging modality used, specificity is high at 82-99%. [1-4] In other words, when pelvic LNs are seen as suspicious on imaging, there’s a very high chance they are indeed prostate cancer metastases.
But there are two arguably much more important questions to consider. First, what exactly does N+ mean in prostate cancer staging these days? And second, does clinical LN negativity equal pathological LN negativity (cN- = pN-)?
To refresh your memory, N1 in TNM classification of prostate cancer only refers to any positive regional (pelvic) LNs, where the short axis of the nodes is >8mm on CT. Any positive LNs outside the pelvis are designated M1a (bone scan is the other traditional imaging modality in prostate cancer staging but is of course not relevant for lymph node assessment).
But now we have a new player in this field called PSMA PET, and, to push the sporting analogy further, it’s hitting CT out of the park! Any PSMA avidity in pelvic LNs on PSMA PET is also N1. But we’ll come back to PSMA PET in a moment.
CT
It is well known that CT scanning for LN staging in prostate cancer has been woefully inadequate. Back in 2008, Hovels et al.’s meta-analysis included 18 studies using CT in over 1,000 patients. Pooled sensitivity of CT was 42%. [1] The authors didn’t hide their frustration, stating that CT is “far too insensitive” in its ability to detect nodal metastases and “should not be used in its current form.”
In another study of over 1,000 patients undergoing radical prostatectomy with pelvic LN dissection in 2016, Gabriele et al. found the sensitivity of CT to be just 8.8% and that it provided no additional predictive value over other pre-operative risk factors. [2] Furthermore, the detection of positive LNs on CT is less than 1% when PSA < 20 or ISUP Grade Group < 4. [5-7]
The problem, of course, is that as a result of such low sensitivity, many patients with true metastatic disease to (and/or beyond) pelvic LNs are only being treated locally, without any certainty that all pelvic LNs will be included in their treatments, either by a surgical dissection template or within the radiation field. Furthermore, even if visibly positive pelvic LNs are effectively treated themselves, they portend a high risk of microscopic disease, not visible on any current imaging modality, further afield.
Risk calculators
Due to CT’s poor sensitivity in pelvic LN staging, risk calculators have been developed using typical clinical risk factors, but these are far from perfect as well. First, previous models were based on systematic biopsy only. And second, whilst the more recent models do incorporate pre-biopsy MRI, which is now the recommended standard of care, and their use could avoid unnecessary LN dissection in more than half of the patients, doing so would miss 2.6% of LN metastases. [8]
PSMA PET
Fast forward to 2021 and we finally have a staging modality with far higher sensitivity: PSMA PET. In their landmark randomised controlled trial proPSMA, Hofman et al. studied 302 men, clinically high-risk patients with biopsy-proven prostate cancer, comparing conventional imaging with CT and bone scan versus Ga-68 PSMA-11 PET. [3] Overall, when including both pelvic LNs and distant metastases, there was an absolute difference in sensitivity of 47%(!) (38% vs 85%) in favour of PSMA PET. A sub-analysis of pelvic LNs was performed, and, calculating from the raw data that was provided, sensitivity of CT vs PSMA PET was 22.5% (9/40) vs 82.9% (29/35), respectively. Even when equivocal LNs were subsequently designated as positive in a sensitivity analysis, the sensitivity of CT increased only to 27.5% (11/40) but that for PSMA PET remained the same at 82.9% (29/35). The specificity of PSMA PET was as high as 98%.
In the same year, Perera et al. published a systematic review and meta-analysis of Ga-68 PSMA PET using 37 articles with 4790 patients, including 5 studies (244 patients) on primary staging. [4] The pooled-per-patient sensitivity of PSMA PET for overall metastatic disease was 77%, but a sub-analysis of pelvic LN sensitivity was not performed. Overall specificity was again extremely high at 97%.
Summary
When pelvic LNs are deemed positive on imaging, they are highly likely to be truly positive if on CT and almost certainly truly positive if on PSMA PET, i.e. cN+ usually = pN+. As specificity is high regardless, this is not much of a clinical issue.
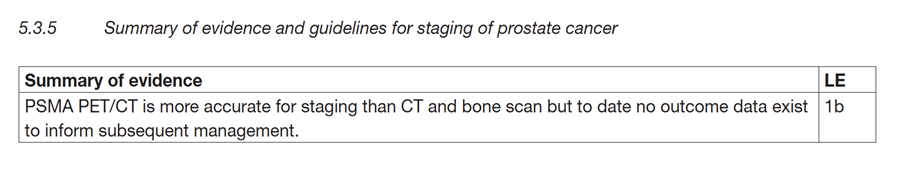
It should be clear, however, from the above recent high-level data that cN- by no means equals pN-. However, PSMA PET is far more likely to detect pelvic LNs than CT. So cN- is far more likely to equal pN- when PSMA PET is used for primary staging of higher-risk prostate cancer. This is reflected in the current EAU Guidelines summary of evidence (see figure 1). [9]
PSMA PET is not yet widely available outside Australia, Germany and the UK, but one question worth considering, given the marked disparity between cN status using CT versus PSMA PET, is whether cN status should be divided accordingly. For example, perhaps pelvic LN positivity on PSMA PET only could be designated cN1a, but cN1b could be considered for CT? This might prove useful in reducing the confusion that now occurs due to the large stage shift caused by PSMA PET’s vastly superior accuracy.
To conclude, PSMA PET represents a major advance in our ability to more accurately stage prostate cancer. As has been the case throughout medical history, the more accurate the staging for cancer, the more likely it is that the optimal management will be chosen. As there are no outcome data based on trials using staging with PSMA PET yet, our dilemma now is: what exactly is that optimal treatment…?
The reference list can be made available to interested readers upon request by sending an email to: communications@uroweb.org.

