Risk stratification and artificial intelligence in MRI-based early detection of prostate cancer
By:
- Dr. Maarten De Rooij (Nijmegen, NL), Department of Medical Imaging at Radboud university medical centre
- Prof. Hein Van Poppel (Leuven, BE), Department of Development and Regeneration at University Hospital KU Leuven
- Prof. Jelle Barentsz (Nijmegen, NL), Department of Medical Imaging at Radboud university medical centre
This article reflects the highlights of the lecture Dr. Maarten De Rooij will be giving during “Thematic Session 16: How machine learning is transforming diagnostics” at EAU21 Virtual. This session takes place in Virtual room 5 on Sunday 11 July, 15.00 – 16.00 CEST.
Early detection of prostate cancer
Screening in a formal sense is not used for prostate cancer (PCa). Already in 2012, the United States Preventive Services Task Force recommended against the use of a serum prostate-specific-antigen (PSA)-based screening program for PCa, because the expected disadvantages outweighed the possible advantages [1]. It was advised not to use the PSA test until men would be well informed. Similar recommendations were stated in the European Association of Urology (EAU) Guidelines [2]. However, these recommendations were based on a conventional non-imaging-based diagnostic strategy; a pathway in which systematic transrectal ultrasound (TRUS)-guided biopsies were used to find the cause of the elevated PSA levels, without using risk-stratification tools such as multivariate risk-calculators or prostate MRI.
In recent years, magnetic resonance imaging (MRI) has transformed the PCa diagnostic pathway, based on multiple high level studies [3-7]. Taken together, the evidence indicates that MRI before biopsy can allow one-third of men to avoid an immediate biopsy and reduce overdiagnoses, with 40% fewer clinically indolent PCa and approximately 15% more clinically significant PCa detected. In the recent EAU Guidelines, MRI now plays an upfront role prior to prostate biopsies [8]. If a suspicious lesion is found on MRI, the subsequent biopsy can be targeted.
Given the changes in the PCa pathway with prostate MRI prior to biopsies, a sharp increase is expected in the number of men who will undergo prostate MRI. This will lead to a challenge: providing good image quality and diagnostic accuracy while meeting the demands of the expected high workload. In this article, we provide a brief overview of the possible solutions to this challenge. These include better pre-imaging risk stratification and adaptations of the MRI pathway with shorter and faster MRI protocols. We will also discuss the role Artificial Intelligence (AI) might play in this specific clinical setting.
Strategies to maintain diagnostic high quality and reduce workload
Better upfront patient selection
A first step to overcome this challenge is to use better pre-imaging risk-stratification tools. In an opinion paper by Prof. Van Poppel and colleagues, an intelligible diagnostic pathway with personalised risk stratification was proposed for early detection of PCa in well-informed men as a so-called “PCa Screening 2.0” [9]. By using this pathway, a more favourable balance between the harms and benefits of early detection is expected. The initial step is to use a PSA test in well-informed men, using age-based PSA interval testing. In case of a PSA elevation, men will be further stratified by using risk calculators [10]. If there is an increased risk of PCa, MRI will be performed. Targeted biopsy is only performed in men with PI-RADS 4 or 5 lesions and in PI-RADS 3 lesions with an unfavourable clinical setting (PSA >10 ng/ml and/or PSA density >0.15). Increasing evidence shows that in case of a negative (PI-RADS 1 or 2) or equivocal MRI (PI-RADS 3) without increased risk (PSA level, family history, age, digital rectal examination), systematic biopsies can be avoided [11].
Risk stratification will never be perfect and will have the consequence of missing clinically significant PCa [12]. It is a challenge to find the optimal balance between a more costly pathway with an increased MRI burden and a more affordable pathway with less MRIs and less unnecessary biopsies, but with missing a few more significant cancers. Cost-effectiveness analyses might be helpful for the different stakeholders, such as policymakers and clinicians, in taking well-informed decisions about the best diagnostic strategies [14].
Better radiology workflow
It is evident that with the changing guidelines there will be an increase in the number of men who will have a prostate MRI. This will lead to an increased pressure especially on the regular radiology programme. One of the solutions is to shorten and simplify prostate-MRI protocols. The omission of a dynamic contrast-enhanced MRI (DCE), resulting in a so-called biparametric (bp)MRI, results in shorter scan times and thus decreased capacity problems. Emerging evidence shows that omitting contrast series does not necessarily lead to missing clinically significant PCa [16]. The most important caveats for the bpMRI protocol are that the studies that have been performed to date have been carried out in expert centres with high-quality scans. Especially in less experienced readers, DCE can be of added value as it can reduce uncertainty, detect more significant cancers, and serve as an extra ‘safety net’ [21].
The role of Artificial Intelligence in the diagnostic pathway of prostate cancer
Artificial Intelligence (AI) can potentially improve the diagnostic quality and reduce the workload. AI is a rapidly emerging technology and has gained massive interest in medical imaging research, mainly in a preclinical setting [22, 23].
AI does not only have the potential to improve the detection of clinically significant PCa, which is generally considered as the most obvious benefit, but can also play a role in the other steps in the diagnostic pathway of PCa: from MR-image acquisition to generating the radiology report (see figure 1).
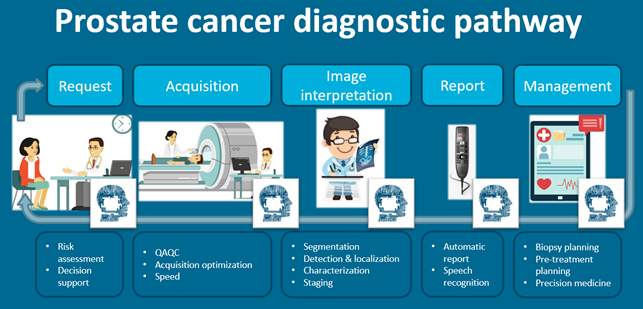
Figure 1: Artificial Intelligence can potentially play a role in all parts of the diagnostic pathway for prostate cancer: from the pre-imaging phase to generating a report. QAQC = quality assurance and quality control
Acquisition
Several studies show that AI can speed up the acquisition of MR images and thus can potentially help solve capacity problems. To date, there are no AI solutions for prostate-MRI image acquisition that can be directly implemented into the clinical workflow; however, in the research field of other body parts, examples do exist. For instance, in musculoskeletal radiology knee MR images can be acquired almost two-fold faster instead of the conventional acquisition technique, with similar or even better image quality [24]. Similar AI solutions for prostate MRI are expected in the future.
Image-quality assurance and quality control
Image-quality assurance and quality control are other potential applications of AI. An international radiological and urological prostate-MRI expert panel considers it mandatory for a radiologist to assess the image quality of each prostate-MR examination and mentions this in the report [25]. To enable this, prostate-image quality (PI-QUAL) assessment criteria for evaluation of a prostate MRI are under development [26, 27]. AI may help to generate a more objective score and to automatically evaluate the image quality during scanning so that technicians may repeat a sequence when it has an inferior quality.
Workflow
Many studies are performed to classify pre-annotated lesions into insignificant versus significant cancer and benign versus malignant lesions [29]. Also, more advanced algorithms are aimed at automated detection and classification of PCa lesions. Promising results are reported. However, it should be noted that most studies concern small cohorts, often without external validation, and have not been validated prospectively in a clinical workflow [30, 31].
Other AI applications
Other AI applications that are of interest are the ones that enable automated detection of ‘normal’ or obvious frequently appearing conditions such as BPH or prostatitis. More research on this topic has been done within breast imaging, where AI is utilised in a screening population to automatically filter out non-cancerous conditions with a high degree of accuracy [32]. Furthermore, AI as a ‘second reader’ could potentially improve the sensitivity of radiologists, which is of particular interest to less experienced radiologists.
Future applications of AI may, based on the combination of different (non-imaging) biomarkers, provide a prediction about which patients will benefit the most from imaging. AI could also predict which patients have a high chance to develop extracapsular extension, or a recurrence, and/or a metastasis, and thus it could allow for a more personalised treatment.
To summarise, the expected rise in the number of prostate MRIs requires solutions that come from different directions. An intelligible risk stratification (i.e. ‘PCa Screening 2.0’) is one of them. Also, other solutions like smarter and shorter MRI protocols need to be explored. In most of these solutions AI can play an important role. In this respect, the abovementioned AI applications have the potential to improve the diagnostic quality of the prostate-MRI pathway and speed up the workflow. However, clinical validation of these tools is needed before fully exploiting their potential.
The reference list can be made available to interested readers upon request by sending an email to: communications@uroweb.org.

