Antimicrobial resistance: How to deal with the pandemic
By Dr. José Medina-Polo (Madrid, ES), Associate Member of the ESIU
This article reflects the highlights of the lecture Dr. José Medina-Polo will be giving during “Thematic Session 12: Emerging threats by infectious diseases” at EAU21 Virtual. This session takes place in Virtual room 3 on Saturday 10 July, 15.15 – 16.15 CEST.
A primary concern for worldwide healthcare systems is the increasing prevalence of antibiotic resistance in hospital and outpatient settings. An estimated 700,000 mortalities occur annually due to unsuccessful antibiotic treatments, and that number is surging. The World Health Organization has declared that antimicrobial resistance is one of the top 10 global public health threats facing humanity. Antibiotics’ widespread use is one of the reasons for the outbreak of microorganisms resistant to antibiotics. The highest antibiotic resistance is reported in low middle-income countries (LMICs), which have the highest antibiotic consumption.
Furthermore, the SARS-CoVID-2 pandemic exacerbated the antimicrobial resistance pandemic, leading to higher consumption of antibiotics. It was estimated that more than 70% of patients hospitalised due to a COVID-19 infection, received antibiotics to treat secondary bacterial infections that represent a significant risk factor for adverse COVID-19 outcomes.
Enterobacteriaceae is among the most frequently isolated bacteria and the main bacteria isolated in urology. To treat infections caused by Enterobacteriaceae, systemic empiric antibiotic treatment with third-generation cephalosporins is commonly recommended. This group of antibiotics is also commonly prescribed for urinary tract infections (UTIs).
Prescription of antibiotics is not the only reason for the increase in antimicrobial resistance. Biocidebased products such as hand sanitisers and surface cleaners could also cause increased rates of antimicrobial resistance.
Cleaning hands is necessary. However, biocide products may affect the prevalence of antimicrobial resistance. Data from our hospital in Madrid which report the increase in antibiotic prescription and antimicrobial resistance during the pandemic are summarised in figures 1 and 2.
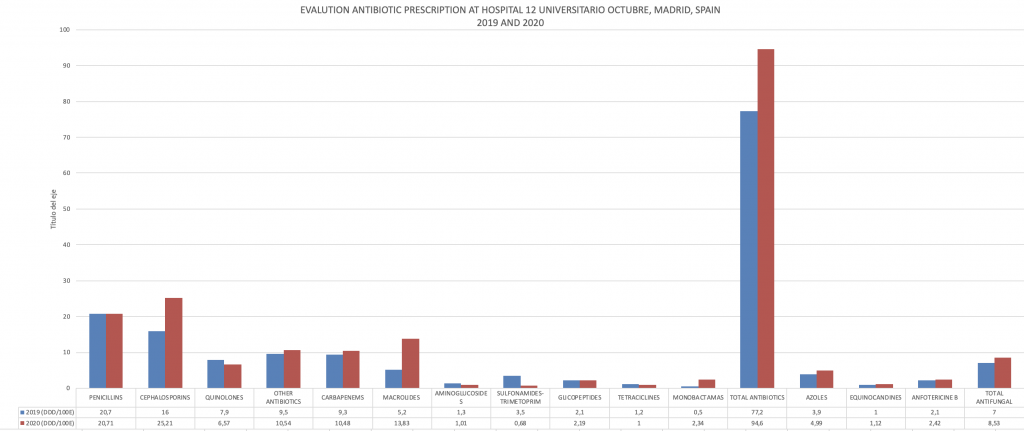
Figure 1: The evaluation antibiotic prescription at Hospital Universitario 12 de Octubre from 2019 to 2020
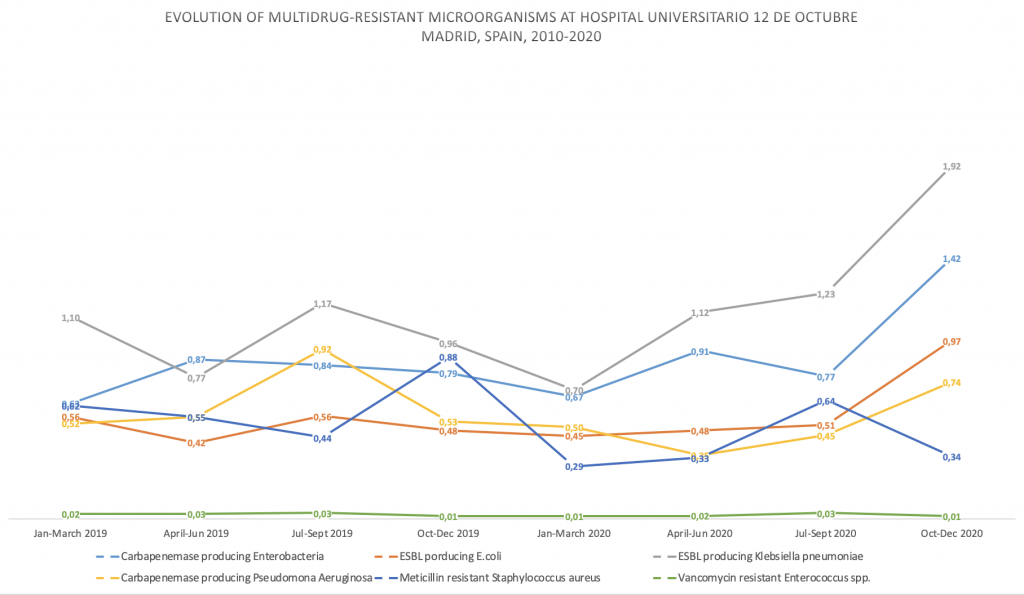
Figure 2: The evolution of MDROs at Hospital Universitario 12 de Octubre from 2010 to 2020
Multidrug-resistant organisms
Although multidrug-resistant organisms (MDROs) are increasing globally; healthcare-associated infections (HAIs) and MDRO infections must be evaluated locally. The revision of incidence must be carried out in each centre due to the variability of resistance with essential differences between continents, countries, and even centres in the same region. Therefore, based on clinical practice guidelines, each centre has to collect its data on the prevalence of MDRO and design protocols to prescribe empirical antibiotic therapy. These measures help optimise treatments and reduce complications and provide a better understanding of the development of resistance.
Urologists must be aware that MDRO infections are common and becoming increasingly familiar. One of the main activities in urology is to assess the characteristics of HAIs through studies such as the Global Prevalence in Infections in Urology (GPIU) and SERPENS which are developed and carried out by the EAU Section of Infections in urology (ESIU).
Treating MDRO infections is a challenging task and may require a multidisciplinary team. When managing patient treatment, urologists have to involve all diagnostic and therapeutic measures. Therefore, it is optimal to have urologists integrated into a multidisciplinary antimicrobial stewardship team comprised of the following:
- Urologists who are experts in the diagnosis and treatment of UTIs
- Nurses with expertise in the diagnosis and treatment of UTIs
- Clinical experts in the diagnosis and treatment of infectious diseases
- Microbiologist
- Hospital pharmacist with a specific training in infectious pathology, antimicrobial optimisation, and calculation of indicators on the consumption of antimicrobials
The team must develop a programme with continuous monitorisation of infections as this has demonstrated that it may optimise the management of infections. According to the standard regulating the implementation of the plan for the optimisation of the use of antimicrobials (PROA) in patients hospitalised in the Hospital Universitario 12 de Octubre from 2019 to 2021, the following measures are recommended:
- Improve the clinical results of patients with UTIs
- Minimise adverse events associated with the use of antimicrobials, including resistances
- Reduce the consumption of antimicrobials, adapt the prescription to the infectious process, and optimise the duration of treatment
- Reduce the incidence of multi-resistant strains
- Make physicians aware of the importance of the correct use of antimicrobials
- Promote the development of research projects
- Promote the improvement of activities related to infection control, the use of antibiotics, and the appearance and spread of multi-resistant strains
- Optimise antibiotic use by ensuring that the appropriate antibiotic is administered at the correct dose and for the right duration
In our department, we have developed a programme with continuous monitoring and prevention of infections (figure 3). The observational study has led to a decrease in the global prevalence of HAIs in patients admitted in the urology ward, from 7.3% in 2012 to figures below 5% in 2019 and 2020.
Figure 3: Continuous monitoring and prevention of infections
Dealing with antimicrobial resistance
However, our data report a high prevalence of MDRO, up to 22.8% of cultures from the urology ward. Urologists have to play an essential role in implementing measures to deal with antimicrobial resistance pandemic in the context of antimicrobial stewardship programs. Antimicrobial stewardship programmes have the following principles:
- Regular training of staff in the best use of antimicrobial agents
- Ensure adherence to local, national or international guidelines
- Regular ward visits and consultation with infectious diseases physicians and clinical microbiologists
- Audit of adherence and treatment outcomes
- Regular monitoring and feedback to prescribers of their performance and local pathogen resistance profiles.
The improvement in the use of antibiotics has reduced the development of antimicrobial resistance, but also reduces the cost associated with hospitalisation and the pharmaceutical cost. An effort to control antimicrobial resistance and prescribe antibiotics more precisely is also recognised as a quality programme contributing excellence to daily clinical care.
The prescription of antibiotics has implications in antibiotic prophylaxis as well. Prophylaxis must be prescribed according to the type of surgery, the degree of contamination in the surgical field, and the risk factors for infections. An adequate indication and selection of prophylaxis are not only associated with a lower incidence of infection but also show lower antibiotic prescription costs.
One of the main issues when dealing with MDRO is the prescription of adequate empirical treatment. Therefore, the management of antimicrobial resistance pandemic in a urological setting requires knowing risk factors for antimicrobial resistance microorganisms isolation, which may determine empirical antimicrobial therapy. In urological patients, immunosuppression, diabetes mellitus or high anaesthetic risk (ASA score III-IV), prior urinary infections and urinary catheter in the upper urinary tract are risk factors for presenting MDRO infections. Among urological patients, those with a catheter in the upper urinary tract (ureteral double-J stent, nephrostomy tube or percutaneous internal-external nephrostomy catheter) require special attention and show the highest prevalence of infections due to MDRO.
In conclusion, the urologist must be aware of the antimicrobial resistance pandemic and collaborate in antimicrobial stewardship programmes. The main actions to implement may be summarised in the following points:
- Review antimicrobial prescriptions and recommend adjustment
- Examine the evolution of microbial resistance
- Evaluate the results of the measures implemented
- Update and promote protocols for the treatment of the most frequent infectious conditions to contribute to optimising antimicrobial prescription
- Training of health professionals in the prevention and treatment of infections as proper use of antimicrobials
- Promote research related to infection and the use of antimicrobial
- Prepare an annual report with the outcomes of the indicators obtained, the evaluation of the results and proposal of new measures.
The reference list can be made available to interested readers upon request by sending an email to: communications@uroweb.org.

