Best Abstracts: Glomerulations as marker for IC/BPS?
By Ass. Prof. Yoshiyuki Akiyama (Tokyo, JP)
Ass. Prof. Yoshiyuki Akiyama is one of the authors of the abstract “Are glomerulations still characteristic marker for interstitial cystitis/bladder pain syndrome? Biological evidences from global gene expression and comprehensive immunohistochemical quantification analyses,” which won the second prize in the EAU20 Best Abstract Awards Non-Oncology. This article reflects its highlights.
A Hunner lesion and glomerulations (mucosal bleeding after bladder overdistension) have been considered characteristic disease markers of interstitial cystitis/bladder pain syndrome (IC/BPS) with and without Hunner lesions respectively and play a significant role in the diagnosis and classification of IC/BPS1,2.
Currently, IC/BPS without Hunner lesions with glomerulations is to be diagnosed as non-Hunner type IC in the East Asian guidelines or BPS type 2 in the International Society for the Study of Bladder Pain Syndrome (ESSIC) guidelines. IC/BPS with neither Hunner lesions nor glomerulations is to be designated as hypersensitive bladder or BPS type 1. In the past, some studies suggested that glomerulations could result from increased neovascularisation and abnormal capillary structure in the bladder mucosa, which might be associated with the pathophysiology of IC/BPS3. To date, IC/BPS without Hunner lesions with glomerulations is likely to be regarded as a disorder of the urinary bladder, with obvious pathology such as ‘bladder mucosal bleeding’4. Moreover, bladder-directed treatments such as intravesical therapies (lidocaine, heparin, hyaluronic acid, chondroitin sulphate, or botulinum toxin) or bladder hydrodistension have been applied to patients with IC/ BPS without Hunner lesions with glomerulations. Thus, the presence or absence of glomerulations plays a critical role in the diagnosis, classification, and clinical management of IC/BPS.
However, a recent meta-analysis study revealed that there was no consistent relationship between glomerulations and the diagnosis of IC/BPS5. Moreover, glomerulations did not correlate with symptom severity and were found in patients without IC/BPS and healthy subjects. In this study, we attempted to seek for biological evidence of glomerulations that could shed light on this controversial matter by conducting systemic genomic and histological analyses in patients with IC/BPS with and without glomerulations. For genomic analysis, we sequenced total RNA obtained from the bladder mucosal biopsies of 21 patients with IC/BPS without Hunner lesions, including with11 and without10 glomerulations, and 9 controls of normal bladder. We looked for differentially expressed genes (DEGs) in order to identify significantly enriched genes and biological processes related to glomerulations.
Unsupervised hierarchical clustering analysis using the DEGs was performed to overview the genomic landscape of IC/BPS with and without glomerulations and normal bladder. For histological analysis, we quantified subepithelial lymphoplasmacytic and mast cell infiltration, neovascularisation, and microvasculature by digital immunohistochemical enumeration of CD3, CD20, CD138, human mast cell tryptase, and vascular endothelial growth factor (VEGF)-positive cells as well as CD31-positive microvessels (defined as capillaries or small precapillary arterioles with an endothelial monolayer, an area of 10 to 314 mm2, and an average luminal diameter of 20 mm or less), using Tissue Studio® software (version 3.5, Definiens AG, Munich (DE)).
Consequently, the presence of glomerulations did not affect global gene expression or the degree of subepithelial lymphoplasmacytic and mast cell infiltration, neovascularisation, and microvasculature. IC/BPS patients lacking Hunner lesions showed a similar gene expression pattern to the controls, regardless of the presence or absence of glomerulations.
A total of 46 DEGs were detected in patients with glomerulations. The number was too small to yield reliable results in the pathway enrichment analysis. Therefore, the presence of glomerulations could not be linked to any biological pathways (see figure 1). There were no differences in densities of lymphoplasmacytic and mast cells, VEGF-positive cells, and microvessels detected between patients with IC/BPS and controls, regardless of the presence or absence of glomerulations (see figure 2). These results indicate that glomerulations may be irrelevant to the subepithelial inflammation, neovascularisation, and microvasculature, suggesting that it may not be a pathognomonic feature of IC/BPS.
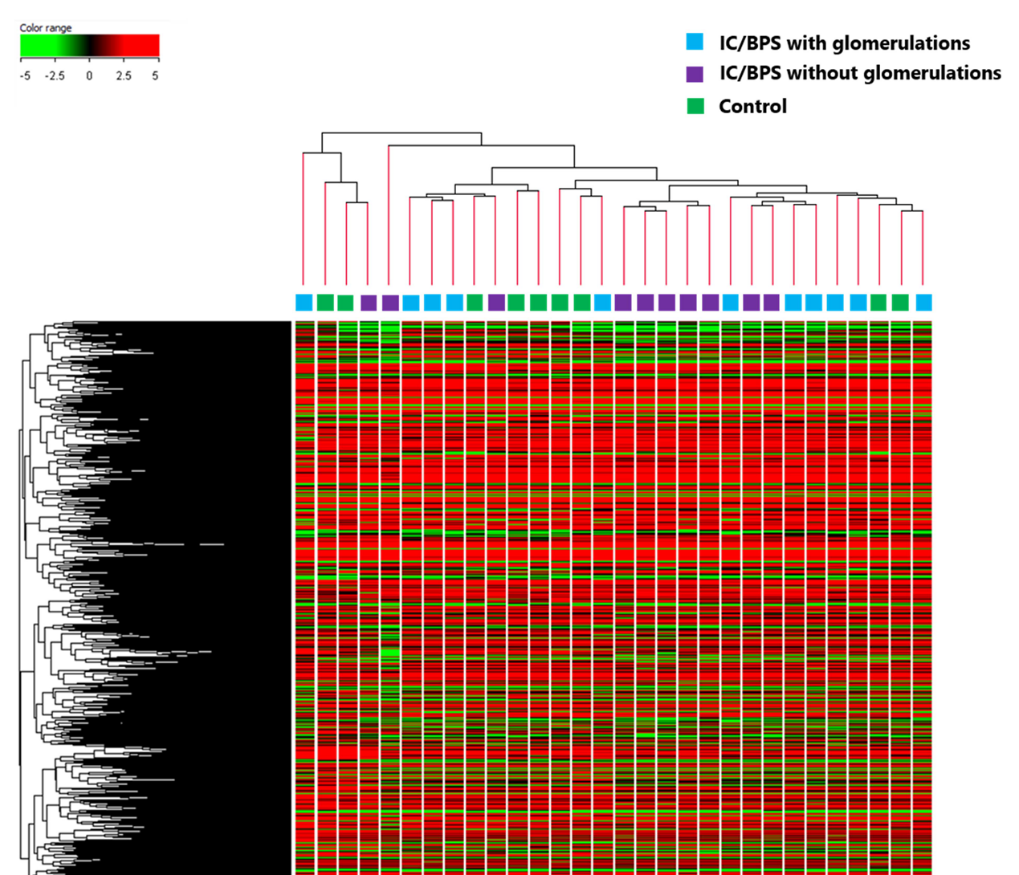
Figure 1: The presence of glomerulations could not be linked to any biological pathways
Collectively, the results of this study could lead to the assumption that a proven, clinically relevant subtype of IC/BPS is the Hunner lesion subtype alone. The Hunner lesion subtype has a definite bladder aetiology and presents with bladder-centric symptoms. Moreover, patients with IC/BPS with Hunner lesions are likely to be responsive to bladder-directed treatments such as fulguration/resection of the lesions and intra-lesion steroid injection6.
Meanwhile, the non-Hunner lesion subtype (potentially regardless of the presence or absence of glomerulations) has little bladder aetiology and presents with widespread, systemic symptoms with a variety of comorbid diseases. This might explain why bladder-directed treatments have limited effects in patients with this subtype7,8,9. However, this study has the limitation of a small sample size, which may not be enough to draw any definitive conclusions. Further biological analyses using larger samples should be warranted to verify the role of glomerulations in the diagnosis and aetiology of IC/BPS.
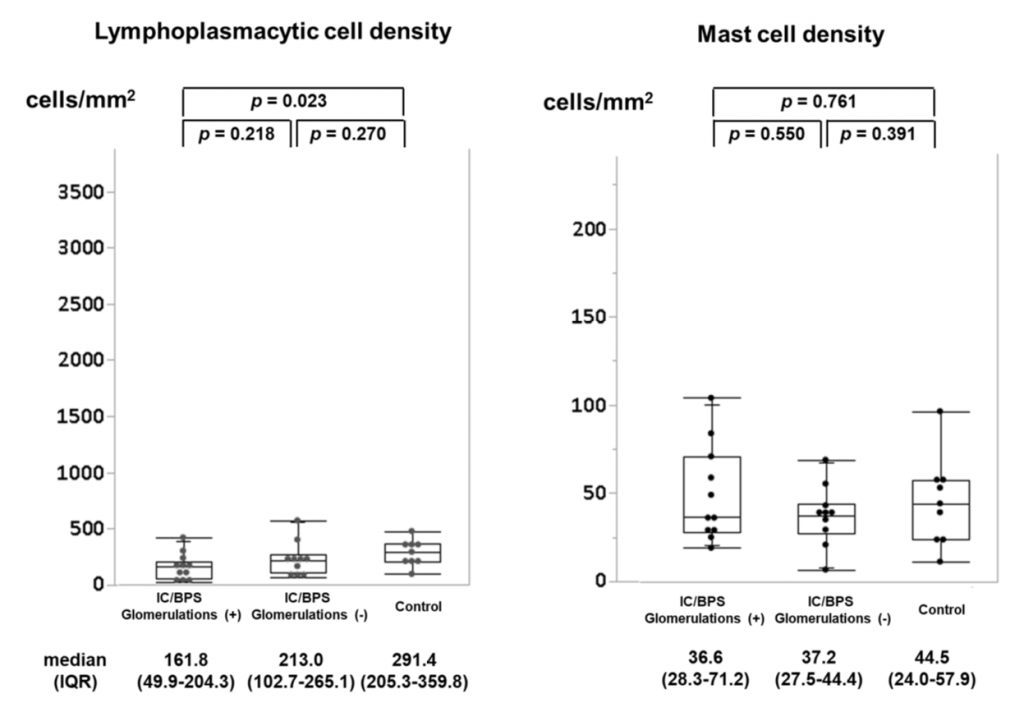
Figure 2A: Lymphoplasmacytic and mast cell densities
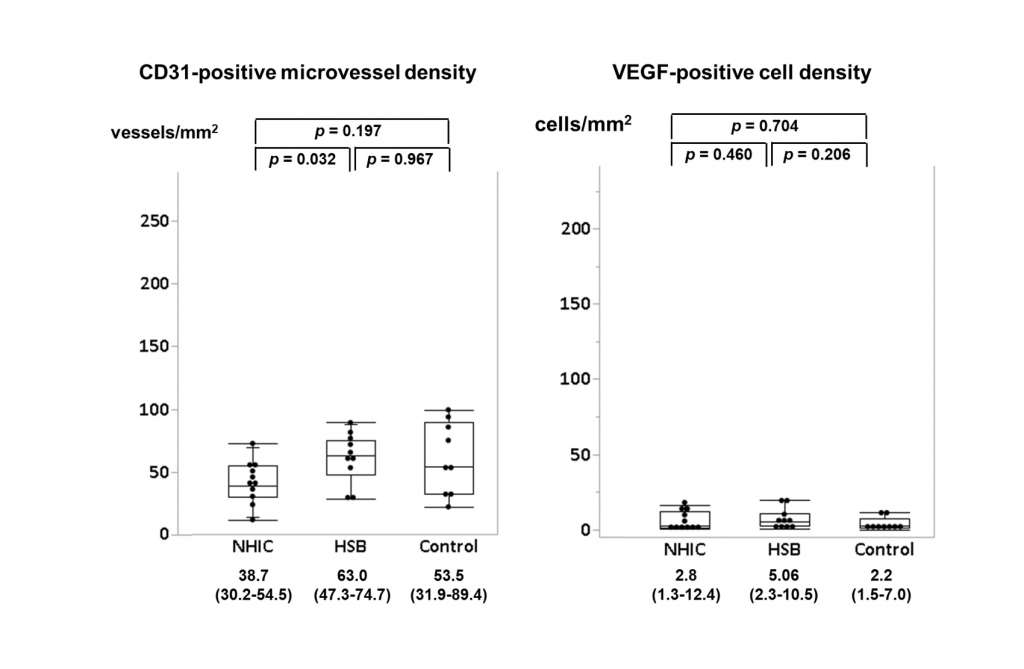
Figure 2B: Microvessel density and VEGF positivity
In conclusion, the current study demonstrated that in IC/BPS without Hunner lesions the presence of glomerulations did not make a difference in global gene expression, densities of subepithelial inflammatory infiltrates and microvessels, and degree of neovascularisation. Glomerulations may not be a phenotypic feature of IC/BPS. It may be about time to revisit the definition, diagnosis, and classification of IC/BPS. Proper subtyping and an accurate understanding of the pathophysiology based on clinical and basic research findings is the only way to achieve better clinical management and future research progress.
The reference list can be made available to interested readers upon request by sending an email to: communications@uroweb.org.
Sign up now for EAU20 Virtual to attend Ass. Prof. Akiyama’s presentation on Saturday 18 July!

