Is there a diminishing role for a re-TUR in NMIBC?
Non Muscle Invasive bladder cancer (NMIBC) is histological diagnosed and treated at the same moment by resecting the initial tumor via the transurethral route (TUR).
The pathological examination of the collected tissue is of importance to stage and grade the disease properly. This information is needed for an accurate treatment plan afterwards. First of all, the important distinction between NMIBC and muscle invasive bladder cancer can be made. In case of NMIBC, together with all collected information at the time of the TUR, the risk of recurrence or progression of the disease can be predicted. For this purpose, the EORTC risk tables take into account, besides stage and grade, the tumor diameter, the amount of tumors, the occurrence of carcinoma in situ (CIS) and whether the disease is primary or recurrent1. On the basis of this risk calculation, an advice on adjuvant treatment is based, according to the EAU guidelines on NMIBC.
In this respect, the T1 and Grade 3 tumors together with CIS are most prone to recur and progress, making the recognition of these stages and grades even more important compared to lower stages and grades. This makes adequate resection combined with accurate pathological examination a key process. But how adequate can we be at both these topics at the same time? A thorough electrical loop resection and fulguration of all vital tumor tissue can be very successful to treat the tumor without the capability to collect proper tissue for PA investigation due to coagulation artifacts. The other way around is also true: beautiful specimens incorporating basal layer and detrusor muscle do not guarantee a complete resection of all tumor tissue.
In high-risk patients (T1 and/or G3), a resection within six weeks after the initial TUR is advised to restage the tumor. In reports on re-TUR, residual tumor tissue was found in up to 50% of patients, suggesting that a complete TUR in these patients is difficult to achieve, while upstaging to muscle invasive disease is described in even 30% of patients in some series5. But very recently, based on combined data of 2451 high-risk NMIBC patients from several centers, a retrospective analysis by Gontero et al. showed strong arguments to believe that after a good TUR, judged on the basis of finding detrusor muscle in the specimen, a re-resection in case of T1 or G3 disease does not alter the outcome of the disease.
The quality of a resection, however, differs among centers. In patients with comparable characteristics treated in seven different EORTC studies, Brausi et al. showed a variation in recurrence rates at the first follow-up cystoscopy after surgery among the different centers, even after taking into account patient characteristics and the use of adjuvant intravesical chemotherapy. In patients with solitary tumors the best center had a three-month recurrence rate of 3.4%. In patients with multiple tumors the highest three-month recurrence rate was 45.8%. Some of these three-month recurrences could be true recurrences, but the majority of these lesions were considered to be tumors missed at the initial resection. In other words, the statistically significant difference could not be explained by factors other than differences in the quality of surgery.
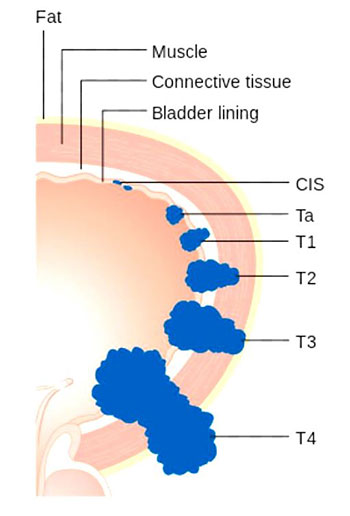
Diagram showing the T stages of bladder cancer
(Photo: Cancer Research UK / Wikimedia Commons)
Knowing how to perform the TUR and teaching someone else to do it are two different things. For this purpose, a complication based study was performed by Pycha et al. In 2003, after a two-year period, their attempt to implement a structured training program did not achieve the desired results: a complication rate of 16% was observed. After another two years continuing this teaching program, the complication rate diminished to 6.1%. Other data about a structured and repeated course on the technical and oncological aspects of the TUR procedure by Brausi et al., showed an increase of quality: the three-month recurrence rate for both residents and staff members decreased significantly (from 8% to 3% for staff and from 28% to 16% for residents), while the presence of muscle in the specimen increased from 50% to 80% overall.
Quality procedure: a crucial role
A transurethral resection of a bladder tumor is an oncological procedure of which the quality is linked to chances of recurrence and progression in case of NMIBC. Introduction of training programs for TUR lead to better resections. A re-TUR is at least indicated in high-risk patients without detrusor muscle present in the specimen, or in a recognized incomplete resection, leading to a motivated selection of patients for this procedure.
Author:
Dr. Jorg Oddens, Department of Urology Jeroen Bosch Hospital, ‘s-Hertogenbosch (NL)

