Is Gleason 6 cancer?
The Gleason score has been the universal grading system for prostate cancer for half a century. In the late 1960s, Donald Gleason (1920-2008) developed his ‘classic’ grading system, which was solely based on the classification of tumor growth patterns and is unique in taking account of tumor heterogeneity.
In 2005 the International Society of Urologic Pathology (ISUP) significantly modified the Gleason grading system. This modification resulted from alterations in clinical presentation and pathological diagnosis of prostate cancer in the preceding 40 years; in Gleason’s day prostate cancer was commonly discovered at a late stage or incidentally at transurethral resection for hyperplasia, since Prostate Specific Antigen (PSA) was only introduced in the late 1980s. Immunohisto-chemistry for basal cells was not included in the pathologic diagnosis of lesions suspicious for prostate cancer at that time. Many closely packed, slightly atypical glands originally classified as Gleason grade 1 or 2 probably represented atypical adenomatous hyperplasia since immunohistochemical staining for basal cells is a prerequisite for differentiating these lesions. In November 2014, the ISUP updated the Gleason grading system again with relatively minor changes in relation to the 2005 modification.
With the modified Gleason grading system the criteria for diagnosing Gleason score 6 prostate cancer became more strict and uniform. As a result of the Gleason grade modification, almost half of ‘classic’ Gleason score 6 tumors on diagnostic biopsies are upgraded to ‘modified’ Gleason score 7. Since the introduction of the modified grading system, several studies have demonstrated very low (<1%), if any, metastatic potential of Gleason score 6 prostate cancer at radical prostatectomy. Considering the minimal chance of metastasis or disease-specific death, the question has been raised whether Gleason score 6 tumors should be considered ‘cancer’ at all.
From a pathologic point of view, the answer to this question is straightforward: Gleason score 6 is cancer. Gleason score 6 shares pathognomic microscopic features with Gleason score 7 to 10 prostate cancer, such as infiltration between pre-existent benign glands, absence of basal cells, presence of prominent nucleoli and perineural invasion. In addition, extra-prostatic expansion and positive surgical margins occur in up to 20% of Gleason score 6 cancers at radical prostatectomy, and are associated with post-operative biochemical recurrence in 10% of cases (Figure 1).
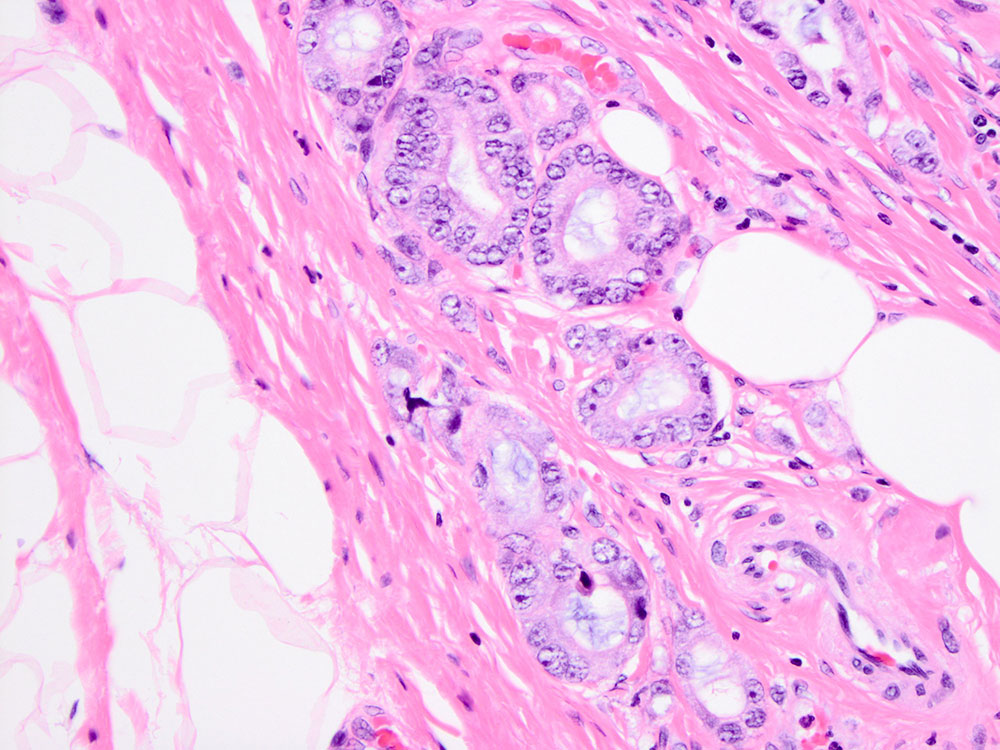
Figure 1: Gleason score 6 prostate cancer glands with expansion into extra-prostatic fat tissue (pT3). Hematoxylin & Eosin, 200x
Despite these arguments, it might still seem attractive to label Gleason score 6 not as cancer but as a lesion of low or indeterminate malignant potential. However, one should realize that the studies demonstrating excellent outcome of Gleason score 6 cancer all involved radical prostatectomy specimens with post-operative adjuvant therapy in case of recurrence. In contrast to Gleason score 6 at prostatectomy, 2% of patients with Gleason score 6 prostate cancer on diagnostic biopsy develop metastasis or die from disease.
It has been known for a long time that the Gleason score at biopsy is lower than the actual Gleason score at radical prostatectomy in up to 20% of cases. This could explain the potential for aggressive behavior of tumors with Gleason score 6 at biopsy. Finally, Gleason grading in daily practice is unfortunately subject to inter-observer variation. Distinguishing Gleason score 6 from Gleason score 7 with ill-formed and fused growth patterns can be particularly problematic, leading to false reassurance or overtreatment of prostate cancer patients.
Pathologic Gleason grading is an important parameter for optimal treatment of individual prostate cancer patients. While many patients with Gleason score 6 prostate cancer are eligible for active surveillance, active treatment is generally preferred for Gleason score 7 tumors. Considering the excellent prognosis of Gleason score 6 prostate cancer, the question arises whether subpopulations with good prognosis can also be identified within the large cohort of Gleason score 7 prostate cancer patients.
Microscopically Gleason score 3+4=7 is composed of well-delineated malignant Gleason grade 3 glands and Gleason grade 4 epithelial structures which encompass a heterogeneous group of growth patterns including so called ill-formed, fused, glomeruloid and cribriform structures. Recently, we and others have shown that Gleason score 7 tumors with cribriform growth, representing 20% of tumors, have a significantly higher risk for biochemical recurrence and metastasis after prostatectomy and radiation therapy. In addition, expansion of prostate cancer within pre-existent glandular structures, called intraductal carcinoma of the prostate (IDC-P), has been shown to represent an adverse feature in disease outcome (Figure 2).
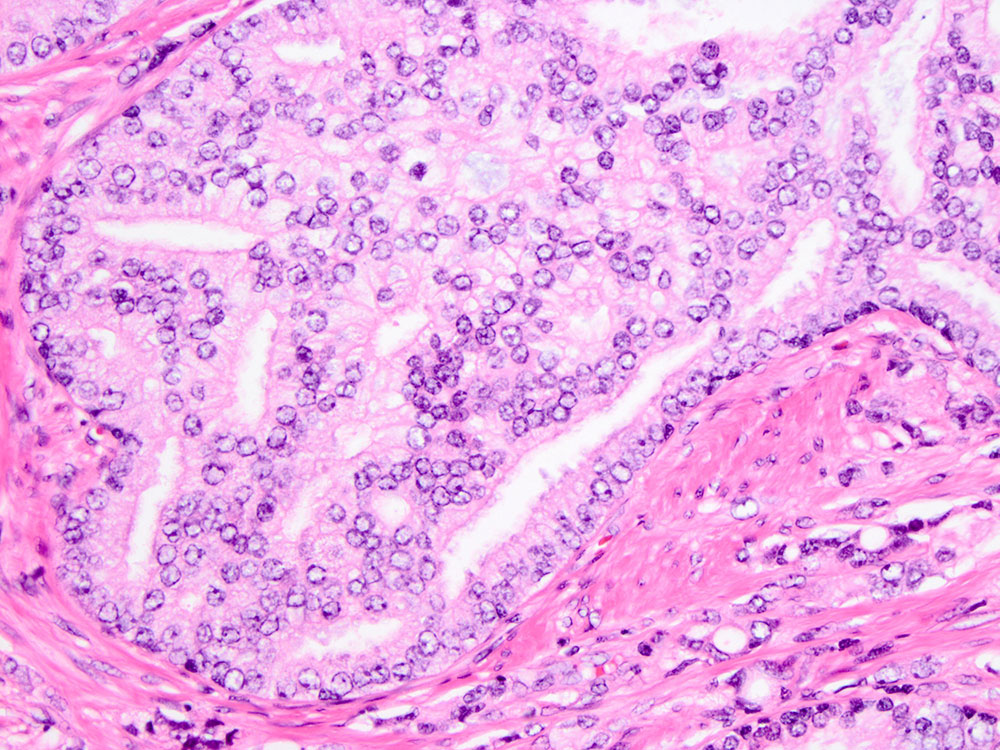
Figure 2: Intraductal carcinoma of the prostate (IDC-P) is an aggressive prostate cancer feature. IDC-P is characterized by large cribriform proliferations of malignant epithelial cells within pre-existent prostate glands. Hematoxylin & Eosin, 200x
Formally, IDC-P is an adjunct tumor characteristic, not being part of the Gleason grading system. Cribriform Gleason grade 4 prostate cancer and IDC-P are closely related; morphologically they can only be separated based on the presence (IDC-P) or absence (cribriform growth) of basal cells, and both lesions often co-exist. In a group of more than 1000 diagnostic biopsies, we have shown that presence of cribriform growth or IDC-P is an independent parameter for diseasespecific death in all Gleason score subpopulations.
Since presence of invasive cribriform or intraductal carcinoma is indicative of aggressive tumor behavior, to what extent do Gleason score 3+4=7 prostate cancer patients without these features differ clinically from Gleason score 6? If patients with invasive cribriform growth and IDC-P are excluded, we found that Gleason score 6 and 7 prostate cancer on biopsy have statistically similar rates of post-operative biochemical recurrence and disease-specific death.
This group of Gleason score 7 cancers consists predominantly of ill-formed and fused malignant glands, which are particularly associated with inter-observer variability in prostate cancer grading. If validated by other groups, these findings might well affect future therapeutic strategies for prostate cancer. Presence of invasive cribriform Gleason grade 4 prostate cancer or IDC-P is indicative of aggressive biological potential and should prompt active treatment. On the other hand, Gleason score 3+4=7 prostate cancer patients without these features might be candidates for active surveillance since their outcome is not statistically different from Gleason score 6 cancers.
In conclusion, Gleason score 6 is prostate cancer but with low potential to metastasize. Invasive cribriform and intraductal carcinoma are aggressive prostate cancer features, which might affect therapeutic stratification of Gleason score 7 prostate cancer patients.
Author:
Dr. Geert van Leenders, Department of Pathology Erasmus MC, Rotterdam, Rotterdam (NL)

