Male LUTS/BPO surgery: Beyond the knife
“Some retrospective article and editorial comments suggest that delayed surgery with medical therapy resulted in poorer outcomes, however we do not have a single prospective study that has investigated the impact of long-term medical treatment and delayed surgical management on patient-important outcomes”, stated Prof. Kari Tikkinen (FI) in his presentation, “The optimal timing for BPO relief surgery: Do we operate too late?”.
In his opinion, delayed surgery probably does not lead to poorer outcomes if you select your patients appropriately. “But if delayed too long, there is risk of poor detrusor function in some patients. The three reasons I believe for this are delayed patient presentation (we need to inform them better), the patients’ fear of the surgery (they are too risk-diverse), or our own wrong decision-making. So clearly there is room for improvement in identifying high-risk patients.”
According to Prof. Tikkinen, evidence suggested that men who report more bother from moderate LUTS vs men that report less bother from moderate LUTS are more likely to benefit from prostate surgery. “Predictors of successful surgery include higher symptom scores, especially voiding, a bladder outlet obstruction index (BOOI) >48, a bladder contractility index (BCI) >123, a maximum flow rate (Qmax) <10 ml/s, fewer or no comorbidities and under the age of 74 yrs. Low scores predict failure from surgery, suggesting preventive TURP (transurethral resection of the prostate) is not a good idea.”
“Patient preferences are the key when deciding on BPO surgery timing because they understand their symptoms and bother. Men tend to take the less risky options and will tolerate symptoms to avoid risk, but this changes as bother increases. It is important to avoid chronic damage to the detrusor and possible renal impairment. Prognosis needs to be discussed and understood by the patient, especially the high-risk ones.”
Persistent LUTS after surgery
In a trouble-shooting session on persistent LUTS after BPH surgery, Prof. Giorgio Russo (IT) delivered a state-of-the-art lecture on the reason/pathophysiology behind this ongoing medical dilemma. “Research suggests that after BPO surgery, approximately 61% of patients still have persistence of LUTS.” He elaborated on the mechanical stretch and gene expression in human bladder smooth muscle cells, as well as the consequences of NGF (nerve growth factor) in relation to overactive bladder (OAB), bladder sensitivity and neuroplasticity.
“To investigate the cause of these persistent LUTS symptoms you must consider the age of the patient (>70 yrs), and the medical history, including diabetes or cardiovascular disease, medication use (as well as anti-cholinergic drug use).”
Prof. Russo’s shared statistics (Jan 2022-Dec 2022) from his own clinic, “LUTS persistence one month after Rezūm included 49% OAB, 27% burning, 16% perineal pain and 8% blood spot.”
On the same topic, Prof. Marcus Drake (GB) presented details on the role, indications and interpretation of urodynamics. He asks the auditorium, “Do we have a problem? Rather a lot of patients don’t actually improve their symptoms after surgery, with IPSS (International prostate symptom score) unchanged after surgery.”
He indicated that LUTS may persist because of inadequate relief of BOO (bladder outlet obstruction), a problem in surgery, storage LUTS/Nocturia, an error in the baseline assessment or the baseline assessment was interpreted incorrectly. “Urodynamics is part of the pathway to predict outcome of further surgery. Many do not do the tests, or verify Qmax, BOOI, or BCI results given by the equipment, or the equipment is not maintained, and this deeply affects the choice of treatment.”
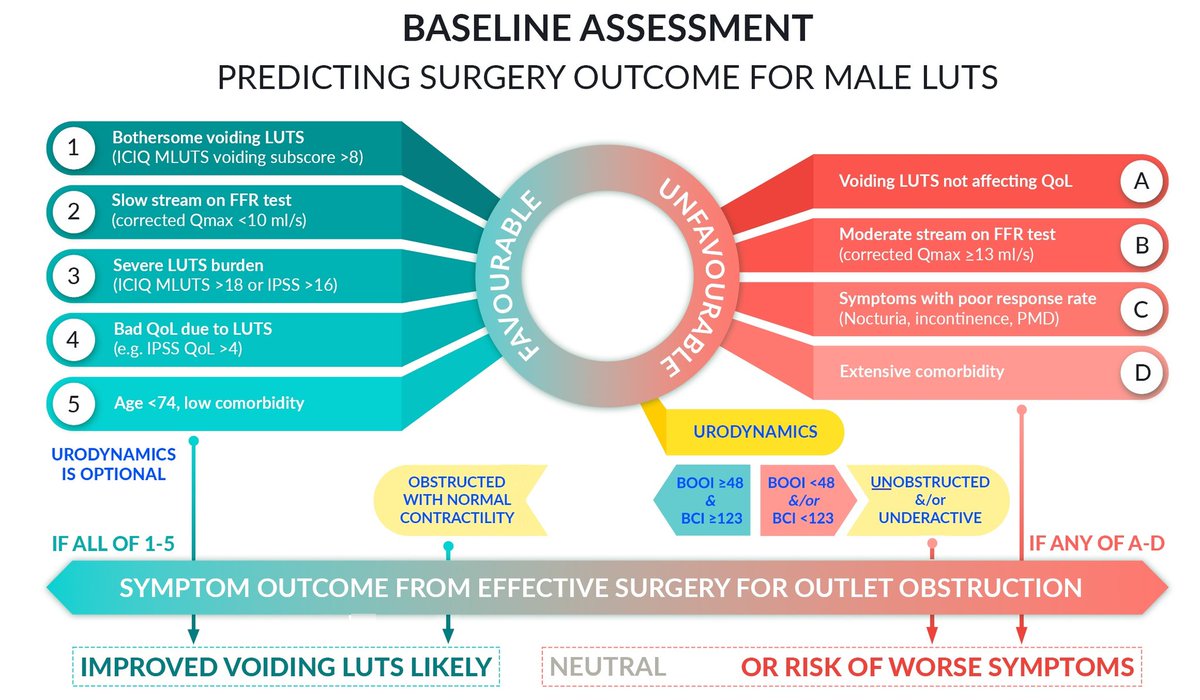
Prof. Drake cited an abstract that was presented at EAU23 (A0026: Predicting prostate cancer surgery outcomes in men with lower urinary tract symptoms to derive symptom score and flowmetry thresholds), and shared graphics of the baseline assessment model he recommends to use in predicting surgery outcomes for male LUTS. He also stressed the use of quality testing at International Continence Society standards, and to review the type of LUTS and which one(s) affect quality of life.
Also included in this session was a case presentation on large prostates and what the best treatment options are, as well as a cross-fire debate on the optimal treatment of persistent OAB symptoms after a good de-obstructive surgery. To (re)watch the full presentations, please go to EAU On Demand on the Virtual Platform

