Looking into the future of treatments for advanced bladder cancer
Scientific efforts of the last decade have produced several novel diagnostic and therapeutic opportunities for patients suffering from muscle-invasive bladder cancer (MIBC) and metastatic disease. “Plenary session 3 – Advanced bladder cancer in 2021: Going forward?” looked into the future of advanced bladder cancer treatment. Chaired by Prof. Dr. Maria De Santis (DE), Prof. Joan Palou (ES), Prof. Morgan Rouprêt (FR), and Prof. Arnulf Stenzl (DE), the session went into technical advances, personalised and targeted therapeutical strategies, and more.
In these times, looking into the future of advanced bladder cancer treatment means looking at the impact of COVID-19 first. Thus, Prof. James Catto (GB) kicked off the session with his state-of-the-art lecture “Safe and optimal management of MIBC in the time of SARS-COV-2.”
“Of our three main cancers [bladder, kidney, and prostate cancer, Ed.], it appears bladder cancer may be the most affected, probably because it is the most aggressive,” Prof. Catto said about the impact of COVID-19 on the survival rates due to treatment delays, citing a study in The Lancet. “[In comparison with the earlier COVID-19 waves], we now have much better risk knowledge. It’s now a case of learning to manage surgery and COVID-19 as it becomes endemic.”
“In terms of cure [for MIBC], we have two choices: surgery or radiotherapy,” Prof. Catto said, then going on to present the pros and cons of each of these approaches in light of COVID-19 (see figure 1).
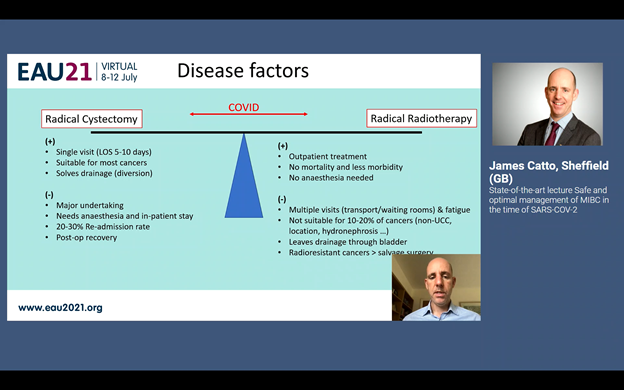
Figure 1: The pros and cons of radical cystectomy versus radical radiotherapy in light of COVID-19.
Molecular markers to decide treatment for MIBC
The second state-of-the-art lecture was given by Prof. Lars Dyrskjøt (DK), who answered the question of whether we can use molecular markers to decide treatment for MIBC. One of his conclusions was that, “ctDNA has many opportunities across the patient disease course to inform clinical practice.” He expounded, “It can be used for tracking minimal residual disease after radical cystectomy, for monitoring response and resistance during, for instance, neo-adjuvant chemotherapy (NAC) and immunotherapy, and for identifying novel actionable targets in metastatic urothelial carcinoma (mUC).”
Prof. Dyrskjøt illustrated his point of the opportunities ctDNA provides by adding two schematic overviews of how ctDNA testing can be used for guiding treatment decisions at diagnosis of MIBC and after cystectomy (see figure 2).
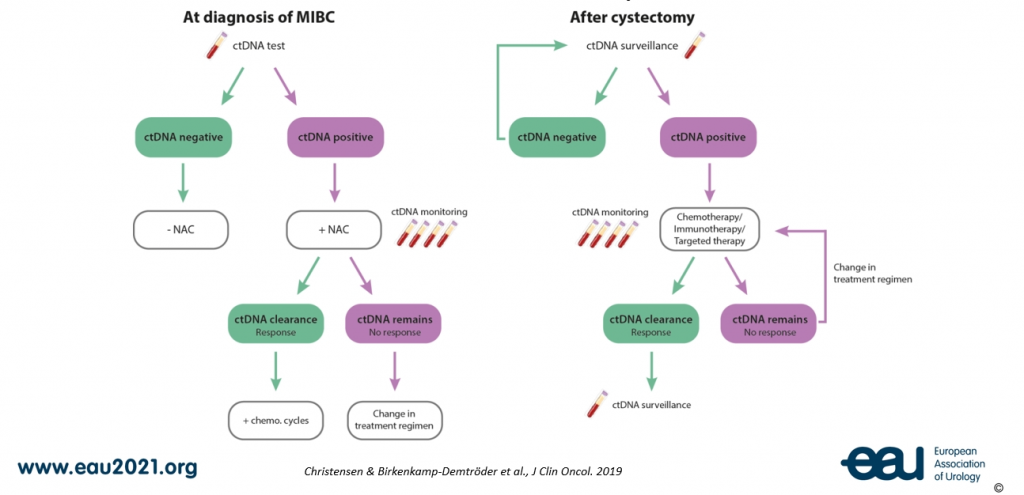
Figure 2: Two schematic overviews of how ctDNA testing can be used for guiding treatment decisions both at diagnosis of MIBC and after cystectomy, respectively.
Immunotherapy in the first-line setting for mUC
The final state-of-the-art lecture of the session was Dr. Enrique Grande’s (ES) “Does every metastatic patient need immunotherapy in a first-line setting?” pertaining to mUC. Dr. Grande answered the central question of his lecture with a “probably not” at the start. He ended with a “definitely not.”
There are key gaps that still need to be filled for immunotherapy in mUC (see figure 3). Dr. Grande further expanded in his conclusion, “The real questions are: can we identify those patients who will be extremely sensitive to chemotherapy and who will not be needing immunotherapy in the long term? Can we identify those patients who will be extremely resistant to immunotherapy? Unfortunately, we do not have the answers to these questions yet.”
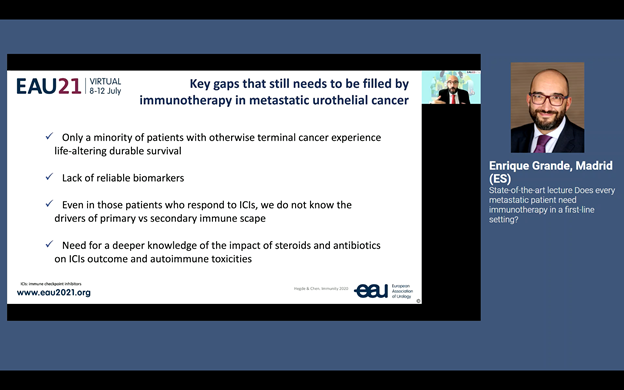
Figure 3.
(Re)watch the full plenary session
Besides the state-of-the-art lectures, Plenary session 3 offered a debate, a clinical case presentation with the oncologist’s and urologist’s point of view, and three more lectures. Keep an eye on the On Demand feature of our Virtual Platform to (re)watch the session as soon as the recording is available!

