Incontinence mesh removal surgery in women
By Dr. Marie-Aimée Perrouin-Verbe (Nantes, FR), Department of Urology, Nantes Academic Hospital & Prof. Hashim Hashim (Bristol, GB), Bristol Urological Institute, Southmead Hospital
This article reflects the highlights of the lecture Prof. Hashim Hashim will be giving during “Thematic Session 01: Guideline Session I: Urethral strictures and female UI” at EAU21 Virtual. This session takes place in Virtual Room 4 on Friday 9 July, 13.45 – 14.45 CEST.
Mesh-augmented surgery for stress urinary incontinence (SUI) in women using minimally invasive surgical techniques and polypropylene mesh were widely used in the 1990s [1] including retropubic (TVT) and transobturator tapes (TOT). Randomised controlled trials showed the effectiveness of mesh surgery compared with conventional surgery, in particular colposuspension. [2] However, the majority of these trials did not report long-term complications.
In a large retrospective study of over 92,000 women in England, complications have been reported in 9.8% of cases at 5 years. [3] Mesh exposure has been reported in 2.7–4.4%, voiding dysfunction requiring surgery in up to 3%, urinary tract infections (UTIs) in 10.7–17.1%, neurological symptoms in 5.4–9.7% [4], and pain in 4.5%, reaching 9% in some series. [5] All these complications may lead to reoperation in 2.2% of cases [6], and most of the time, multiple operations are required before the mesh is entirely removed. [7] Indeed, some authors reported the need for a median of two revision surgeries (range 1-9) to remove the mesh. [8]
Recommended pre-operative assessment
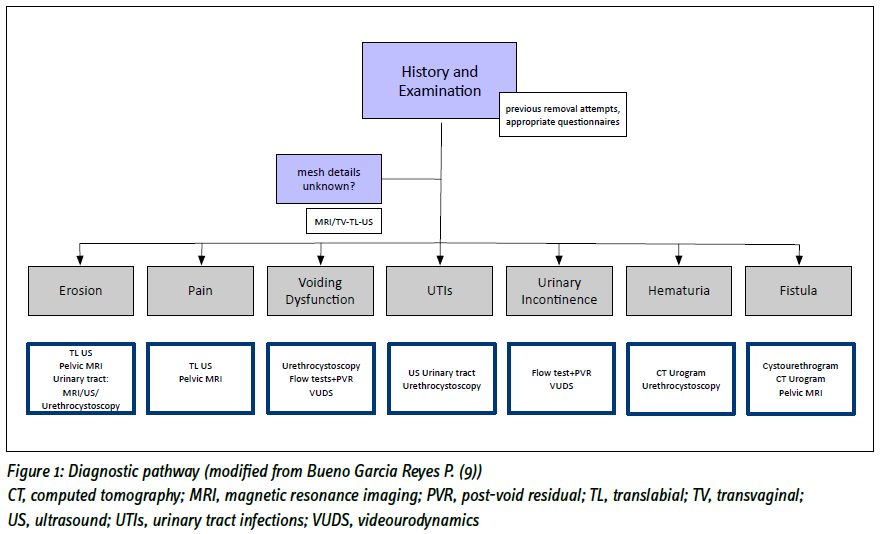
There are currently no guidelines on pre-operative assessment in case of incontinence mesh complications. A complete medical history and examination are needed. Multidisciplinary evaluation is encouraged, especially if there are other symptoms related to mesh such as pain or musculoskeletal issues. [9] There are currently no mesh-specific validated outcome questionnaires. [9] Vaginal and pelvic examination are mandatory as they may reveal vaginal erosion, trigger points for pain or tender areas. We recently published a diagnostic pathway for incontinence mesh complications (Fig 1) [9] and investigations are targeted towards the mesh complication.
Mesh complications classification and standardization
There is a lack of standardization in terminology to describe mesh complications, as well as, surgical mesh removal terminology. IUGA/ICS has proposed a comprehensive calculator. [10] However, this classification can be complex to use routinely and seems to be more suitable for research. Therefore, we recommend making a detailed report with the complete history, the reported symptoms and the results of the clinical examination. In case of mesh removal surgery, a comprehensive and detailed description of the procedure is mandatory including measurement, recording of the length and photos of the mesh removed. [9] This is helpful if further surgery is required and may be useful for medico-legal purposes too.
The terminology proposed by AUGS-IUGA [11] to describe the surgical procedure may be confusing, therefore we proposed to use the following terminology for mesh removal [9]:
- Covering of the mesh with vaginal tissue: this does not involve removal or division of the mesh and only involves dissection of the vaginal tissue and using that to cover the exposed mesh
- Division of the mesh: this involves cutting the mesh without removing any part of it and is usually used in those with voiding dysfunction.
- Partial removal/excision of the mesh: this involves removing only part of the mesh. The site and length of the mesh removed will have to be specified.
- Full removal of the mesh: removing all the mesh from one end to the other.
- Completion removal of the mesh: this is where they had a previous partial removal and the rest of the mesh needed to be removed fully.
Incontinence mesh removal surgery: When and how?
Whatever the complication, a tailored individualised treatment must be proposed to the patients. Before planning surgery, it is crucial to collect the patient’s expectations and goals. Patients must be aware of the benefits and harms of the mesh removal surgery, notably the failure to remove the entire mesh, no change or worsening of the predominant symptom, and the risk of stress urinary incontinence (SUI) recurrence. They also may be aware of the possibility of needing more than one procedure. NICE have developed a patient decision aid for mesh removal [12] which are given to patients.
A multidisciplinary management may be considered, depending on the complication. For example, in cases of pain, pain specialists, psychologists/ psychiatrists and physiotherapists have a key role in patient management. Other surgeons may be involved, depending on the type of complication. For example, orthopaedic surgeons may be included in cases of needing groin dissection for TOT removals or colorectal surgeons may be involved in case of bowel complications. Finally, in the UK, NICE also recommends to discuss all mesh removal surgeries cases in a regional multidisciplinary team meeting. [13]
Vaginal erosion
In case of asymptomatic vaginal erosion, with an area of exposed mesh less than 1cm2, initial conservative treatment using topical vaginal oestrogen for at least 3 months before surgical options are considered may be tried. [13] There is some evidence of a higher risk of failure compared with surgery as an initial step, and up to 59.3% of women managed initially conservatively will eventually need surgical treatment. [9] Surgery may be proposed in case of symptomatic vaginal erosion, or failure of conservative treatment: removal of all the vaginal portion is at higher risk of SUI recurrence than removing part of the vaginal component, however the risk of exposure in the latter is lower. [9] In case of adherent mesh to the urethra and per-operative urethral injury, tissue interposition with Martius labial fat pad graft may be required.
Urinary tract extrusion
Extrusion into the urinary tract requires surgical removal as the mesh can cause infection, lower urinary tract symptoms (LUTS), stones and/or pain. A systematic review including 20 articles, reported that endoscopic treatment is an effective minimal invasive option, with an initial success rate of 67 % for laser excision and 80% for endoscopic excision. [14] However, between 18 to 25% of patients required at least one additional procedure, some of them with an open approach. Moreover, this technique did not prevent SUI recurrence (around 20% of the patients). [14] In cases of non-endoscopic management, the risk of SUI recurrence is higher with complete than with partial mesh removal. [13] The type of removal has to be discussed with the patient, and risks and benefits discussed carefully. In cases of urinary tract extrusions, it is best that women are managed in specialised centres. [13]
Pain
The incidence of chronic postoperative pain after placement of sub-urethral tape for incontinence varies between 0 and 30% depending on the study. A higher incidence is also observed after transobturator surgery compared with retropubic surgery. [15,16] The chronology of pain occurring after the surgical procedure is a major factor to establish a causal link between surgery, placement of prosthetic material and the patient’s symptoms. [17] A detailed analysis of the patient’s symptoms can then help to define the type of lesion: myofascial, neuropathic, and/or autonomic. Indeed, the pain may be due to somatic nerve lesions or decompensated neuropathic pain, muscle pain due to direct injury or reactive pain, or finally much more diffuse pain accompanied by urinary, gastrointestinal or sexual symptoms in a context of pelvic sensitization. [17,18]
If no mesh abnormality is found, non-surgical treatment is initiated, and if no improvement is achieved, advice from the mesh multidisciplinary team must be sought before any surgical treatment is decided. Trigger point injections with local anaesthetic, as a trial of treatment can be useful and can also help establish an association with mesh. [9] Partial mesh excision may be considered only if pain is related to a specific component of the sling. [9] Therefore, some authors suggest performing groin incision only in patients with associated preoperative obturator neuralgia, for the removal of the prosthetic material and obturator nerve release. [17]
In patients with myofascial pain, section of the material to release excessive tension phenomena, without complete removal, may sometimes be sufficient. [15] However partial removals make future removals of any remnant mesh more difficult due to scarring and retraction of the mesh. [9]
Full mesh removal improves pain in around 60% of cases [9,17] and may reach more than 80% of cases. [19] Persistent pain may be a major cause of dissatisfaction, and patients must be made aware of this risk. In cases of persistent pain after complete mesh removal, the patient should be referred to a pain management centre for global pain management, with multimodal treatments. [17]
Lower Urinary Tract Symptoms (LUTS)
Chronic voiding symptoms is one of the most frequent complication of tapes, with reported rates ranging between 2.8 to 34.7%. [19] If retention is the only complication from sling insertion, sub-urethral mesh division or partial excision may be enough, with high resolution rates after surgery. [20,21]
Laparoscopic or open approach?
Laparoscopic approaches have been published for mesh removals. However, to the best of our knowledge, there are no studies comparing abdominal open versus laparoscopic approaches. In our experience, laparoscopic surgery does not remove the mesh fully in retropubic tapes, especially the supra-fascial/subdermal portion of the mesh, but may be facilitated by using a robot. In the transobturator route, it is often difficult to get the mesh out from within the muscle fibres in the obturator foramen. [9] However, some authors state that obturator nerve release may also be performed via laparoscopic approach to access the pelvic course of the nerve and may be indicated in case of obturator neuralgia. [17]
Outcomes of mesh removals
Functional outcomes
Mesh removal surgery can lead to a complete resolution of symptoms in about 60%-70% [19,21-23] except for chronic storage symptoms (urgency, frequency, urgency urinary incontinence) which may have a lower success rate. The higher success rate is when the mesh removal surgery is indicated for voiding dysfunction. [20] SUI recurrence after mesh removal is a common adverse event, with 20 to 50% of the patients concerned [9,17,24,25], whatever the indication for removal, and is more prevalent in cases of full removal. [24]
Quality of life outcomes
There is a scarcity of data focusing on quality of life, as well as sexual life after incontinence mesh removal surgery. Our results on functional and quality of life outcomes after TOT removal [26] showed satisfaction rate was high (86%). 81% of the patients considered the surgery successful, 93% would still have the surgery if they were in the same situation again, and 95% would recommend this surgery. Moreover, 70% returned to having a sexual life after surgery, with 80% considering it about the same, a bit better or much better than before the surgery.
Conclusion/ implication for practice
Multidisciplinary management is encouraged for patients with mesh complications and joint/shared decision-making is crucial when offering mesh removal surgery using patient-decision aids.
The reference list can be made available to interested readers upon request by sending an email to: communications@uroweb.org.

