What are the limits of nephron sparing surgery?
Renal cell carcinoma (RCC) represents 3% of all adult malignancies. Its incidence has increased over the last decades, around 3.7% per year, probably because of the increase in abdominal imaging performed for other causes.
Most of the increased incidence is due to the detection of small renal masses (<4cm), but even nowadays around a third of patients with RCC still present with metastatic disease. On the other hand in industrialized countries the incidence of comorbidities such as hypertension and diabetes has also increased over the last decades, having a direct impact on the development of chronic kidney disease (CKD), and conveying a higher risk of cardiovascular diseases.
Twenty years ago, the indication for a nephron sparing surgery (NSS) was limited to small renal masses and patients with impaired renal function. During these two decades, the tendency has been to reduce morbidity using minimal invasive techniques like laparoscopy, and to preserve renal function while maintaining good oncologic results; Partial nephrectomy (PN), using minimal or open techniques, have been adopted worldwide and are increasing in number.
Currently, PN has become the standard of care for small renal masses (>4cm); in larger tumors (<7cm) even for tumors >7cm can be considered as an indication when technically feasible1. This increasing acceptance for partial nephrectomy in bigger tumors is related in part to the higher incidence of CKD in this population. Indeed around 25% of patients with RCC present with underlying CKD.
In initial studies, PN for small tumors <4cm demonstrated improved overall survival in comparison to radical nephrectomy. PN in lesions measuring 4 to 7 cm compared to radical nephrectomy have equivalent recurrence-free, CSS and overall survival.
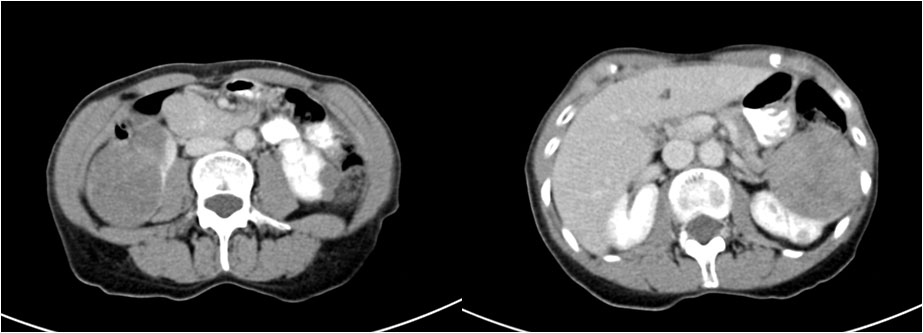
Figure 1: 65-year-old female with bilateral tumor (6.8 in the left side and 4,5 in the right)
For larger tumors, PN has demonstrated feasibility and oncologic safety in carefully selected patients, but those results remain controversial. Those results taken together with the fact that CKD and end stage renal disease (ESRD) impact on morbidity and mortality suggest that PN should be considered the procedure of choice when feasible in renal tumors less than 7cm and in some cases of tumors larger than 7. It seems that the tendency is to perform PN in more and more complex renal mass, with the major objective of preserving as much as possible renal function. So, in this scenario which are the limits for a partial nephrectomy?
Imaging techniques
Nowadays, we have excellent imaging techniques (angioCT scan, with 3D reconstruction) that permit a better anatomical pre-operative planning recognition of the tumor and, consequently, a better surgical plan. In the future we also will get 3D impressions that could help these types of surgeries.
Surgeons have improved surgical abilities (laparoscopic and open) with better instrumentation and optics (3D vision) and the introduction of robotics; at times it looks as if it is now possible to perform almost everything and the sky is the limit.
As previously mentioned, tumor size used to be a limiting factor for partial nephrectomy years ago, but has now evolved into the current treatment of choice for small renal masses and even for tumors < 7cm.
Currently, even tumors larger than 7cm are now safely resected. In a recent paper published by Long et al, in 46 patients with renal tumors bigger than 7cm treated by partial nephrectomy, five and 10 years overall and RCC specific survival were 94.5% and 70.9%.
Influenced by tumor size and location, the concept of warm ischemia time has become important, because the more difficult the tumor is in terms of size, morphology and location, the longer the warm ischemia time. The 30-minute limit is well established in order to avoid irreversible damage to the kidney function. When required, if extra-time is likely, cold ischemia should be considered.
When we analyze results of partial nephrectomies, the achievement of the Trifecta (Warm ischemia time <25, negative surgical margins and no complications) is very important. In a recent study analysing the Trifecta achievement in PN for tumors >7cm compared to tumors between 4-7 were similar.
Lower RENAL score in series was significantly associated with the Trifecta achievement.
Tumor size and location have been grouped in the morphometric scores systems such as the R.E.N.A.L. score, the P.A.D.U.A. score and C-index, in order to get a grasp on the feasibility and predict post-operative complications when planning surgery. When dealing with complex cases and especially a complex mass, options include nephrectomy, ex-vivo partial nephrectomy and auto-transplant.

Figure 2: CT scan after bilateral partial laparoscopic nephrectomy. Post-operative creatinine 1,49: Pathology: papillary renal cell carcinoma Furhman II
Partial nephrectomy in the setting of patients with metastatic disease also plays a role, albeit controversial, due to the importance of renal function preservation, especially in patients with solitary kidney. Limited data are reported on that setting; series of small number of patients reported better cancer-specific survival rates in PN or equal cancerspecific survival than radical nephrectomy.
It is well known that RCC is more frequent in patients on dialysis and this higher incidence persists after kidney transplantation. RCC may occur on native kidneys and in the transplanted one. The treatment of choice in a transplanted kidney should be the same than in the general population; partial nephrectomy should be considered as the first choice to maintain kidney function avoiding dialysis.
In the literature several series have reported the results of partial nephrectomies in transplanted kidneys, with good oncological and functional results.
New concepts
Recently, new concepts have emerged like the enucleation of the tumor in complex renal mass. In a recent paper of 96 tumors treated by simple enucleation, the authors described good results, concluding that enucleation for highly complex renal tumors is an effective treatment, with a potential key role in NSS.
In experienced surgeon’s hands almost everything can be done, but the balance of surgical complications, complexity, renal function preservation and safety oncologic outcomes is very important. And the most important thing for surgeons is to know and set their own limits.
Author:
Dr. Mireia Musquera, Hospital Clínic de Barcelona, Barcelona (ES)

