Plenary Session 4: State-of-the-art lectures overview
Spearheaded by Chair of the EAU Guidelines Office Prof. Dr. Maria Jose Ribal Caparros (ES) and ESOU Chair Prof. Morgan Rouprêt (FR), Plenary Session 04: Perioperative treatment of urothelial cancer in 2022 provided insights and updates on bladder cancer. This article provides a quick overview of the three state-of-the-art lectures which took place during the session.
The presentation “Landscape of current trials with intravesical treatment in high-risk BCG naïve NMIBC” by Prof. Dr. Ashish Kamat (US) kickstarted Plenary Session 4. During his lecture, he underscored that for the purpose of clinical studies, all high-grade tumours should be considered high-risk. “This is not to take away from the EAU Guidelines classification which is good for counselling patients,” said Prof. Kamat. He added that patients with Bacillus Calmette-Guérin (BCG)-naive NMIBC should not be enrolled in a single-arm study; they should be enrolled in a randomised controlled trial (RCT) with a control group.
As an example, Prof. Kamat mentioned that the interim analysis data cutoff of the POTOMAC study has been continuously pushed back due to events occurring at a much slower rate than expected. He stated, “BCG contemporary outcomes are much better than any of us remember.” Prof. Kamat presented data on 542 patients receiving adequate BCG, as defined by the FDA, with a median follow-up of 48 months (Matulay, et al., J. Urol 2021). He said, “The progression rates in high-risk patients are extremely slow. Even in 2022, BCG still remains the treatment to beat.”
In “Lynch syndrome: What urologists need to know”, Prof. Rouprêt stated that Lynch syndrome is the most common familial cancer syndrome that was first described by Aldred Warthin in 1895.
In identifying Lynch syndrome in patients, Prof. Rouprêt mentioned the Bethesda criteria to test tumour for microsatellite instability (MSI), which included colorectal cancer in a patient who is younger than 50 years old, and presence of synchronous or metachronous syndrome-associated tumours regardless of age, to name a few. In addition, he mentioned the Amsterdam criteria, which involved a patient’s three relatives with a Lynch syndrome-associated cancer (e.g. colorectal cancer, endometrial, etc.) wherein one is a first-degree relative of the other two and at least two successive generations are affected; and other indicators.
Furthermore, Prof. Rouprêt presented an EAU Guidelines flowchart in how to identify a patient with Lynch syndrome (see image below).
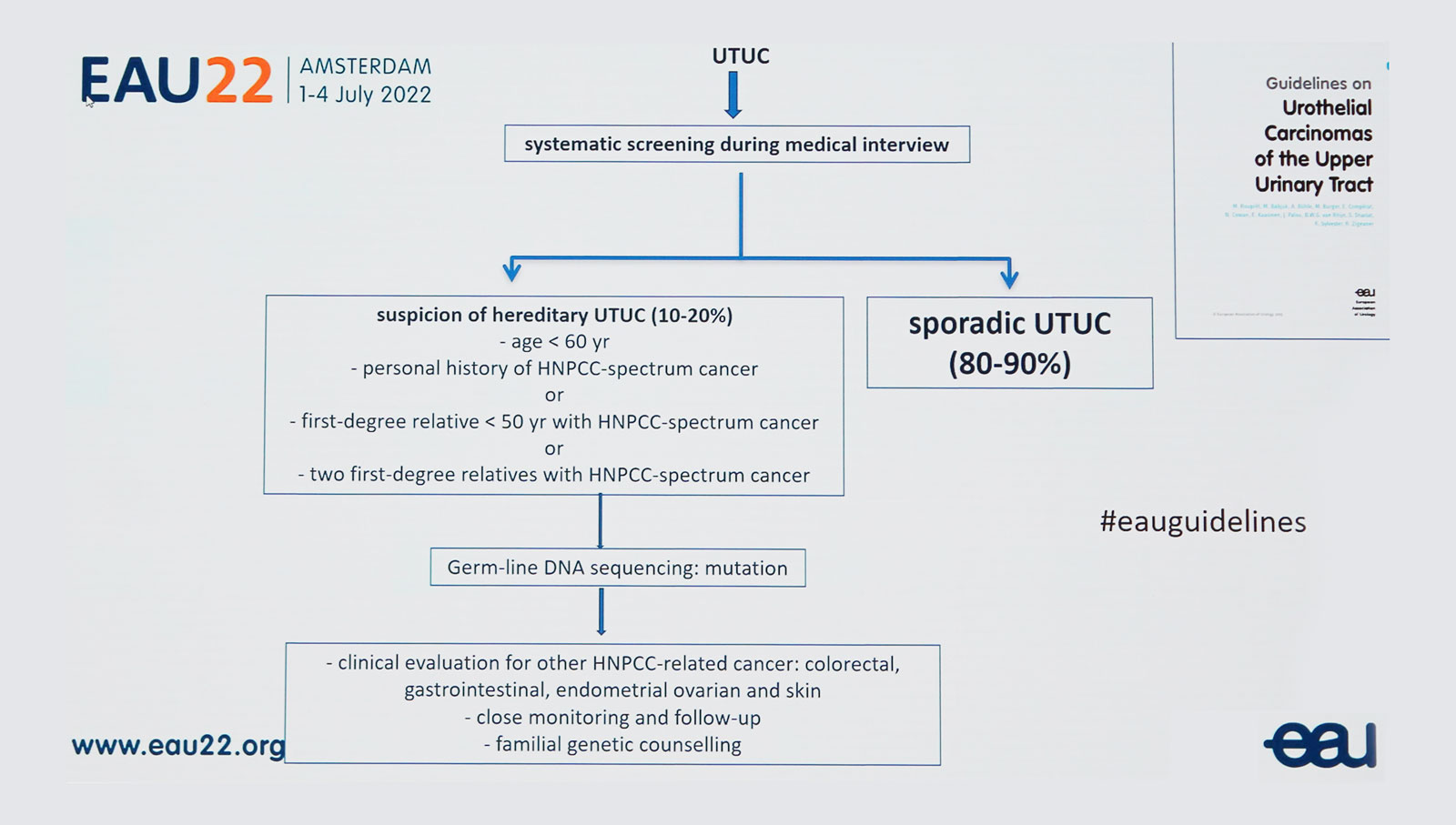
He emphasised that there should be clinical evaluation for other HNPCC (hereditary nonpolyposis colorectal cancer)-related cancer (e.g. colorectal, gastrointestinal, endometrial ovarian, or skin cancer), as well as, close monitoring with follow-up, and familial genetic counselling.
In the presentation “Molecular classification in bladder cancer to guide systemic treatment: ready from prime time?”, Dr. Peter Black (CA) answered this question by stating “Molecular classification in bladder cancer is approaching prime time.” He said that RNA-subtyping is being tested in two prospective RCTs and this will provide a lot more information about treatment, intensification, or alternate treatment. These RCTs are under development to determine value in selecting neoadjuvant systemic therapy.
In addition, the DNA damage repair gene alterations are potentially for the de-escalation of standard therapy. Three prospective RCTs are underway to test the ability of markers to guide bladder preservation after chemo/immunotherapy.
He concluded, “Until then, molecular classification of MIBC is not ready for prime time.”(Re)watch the full presentations of Plenary Session 4 via EAU22 On Demand on the Virtual Platform.

